Dr Chelvin Sng: When should you visit an Eye Specialist (Ophthalmologist) in Singapore?
An eye specialist, or ophthalmologist, is a doctor who diagnoses and treats various eye disorders and is qualified to perform eye surgeries. An ophthalmologist differs from an optometrist, who performs vision tests and prescribes corrective lenses and eyewear.
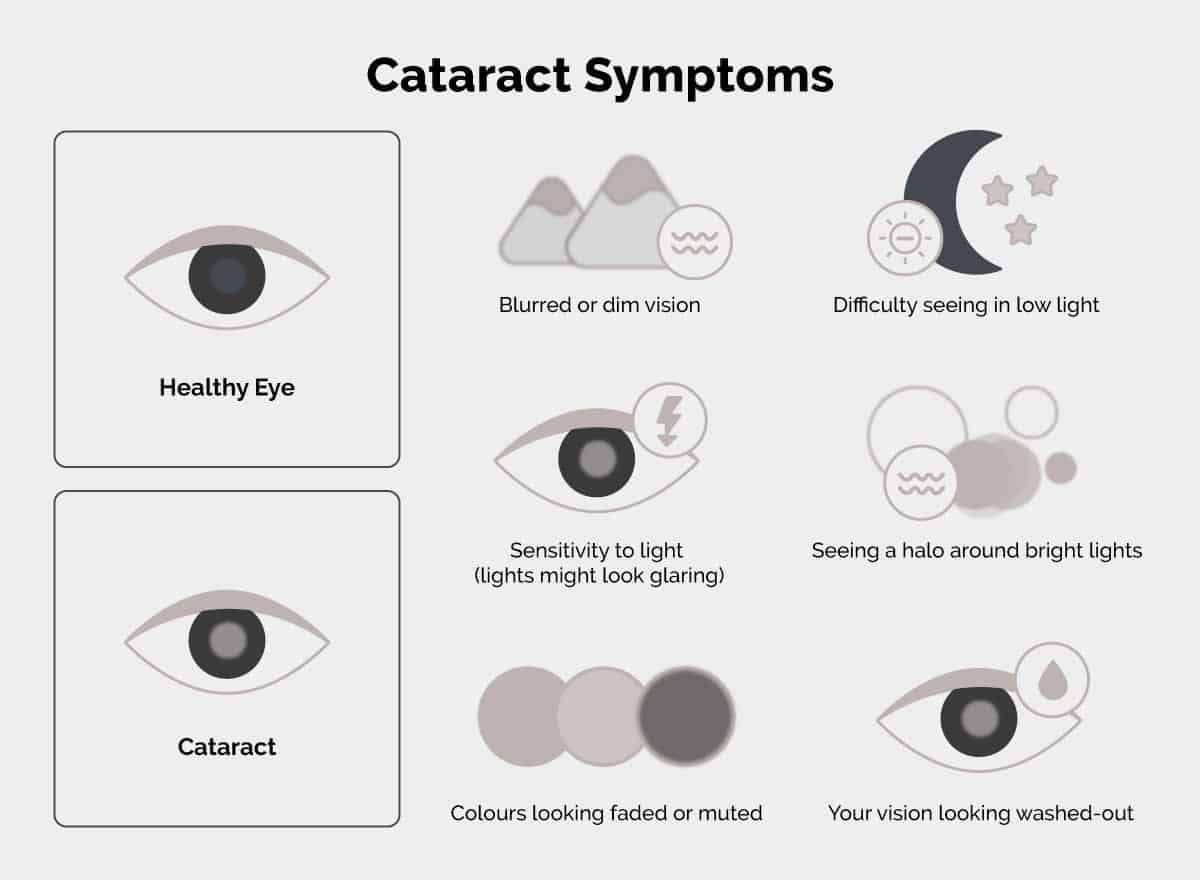
In Singapore, several prevalent eye issues require individuals to consult with ophthalmologists. These include myopia, or nearsightedness, common among children and young adults [1], and cataract, usually associated with older adults [2]. It is important to consult with an ophthalmologist for eye issues and problems such as these, as they can worsen over time and even lead to permanent vision loss.
With Singapore’s ageing population, maintaining eye health is critical as age-related conditions, such as cataract, glaucoma and macular degeneration, become more common. Keep reading to find out what eye specialists do, when to visit an ophthalmologist, and how to choose the right one in Singapore.

Specialised Services by Eye Specialists
Eye specialists in Singapore offer an array of advanced services to address the unique needs of patients. These professionals are equipped to provide medical care beyond routine checkups, ensuring precise diagnoses and tailored treatments.
From managing eye diseases to prescribing medications and performing corrective surgeries, the services typically aim to improve visual function. Catering to all age groups, eye specialists offer specialised pediatric care to help children manage vision issues early. Through their experience, they ensure patients receive comprehensive and personalised attention to manage long-term eye health and improve quality of life.
Here are some services carried out by eye specialists:
Comprehensive Eye Examinations
Eye specialists carry out detailed evaluations to detect conditions like cataract, glaucoma, macular degeneration, and diabetic retinopathy. Comprehensive eye exams and screenings not only preserve vision but also provide insights into a person’s overall health, as systemic conditions like hypertension or diabetes can manifest in the eyes. These include:
- Visual Acuity Test: Measures how clearly you can see at different distances using an eye chart.
- Refraction Test: Determines the presence of refractive errors, such as myopia, hyperopia, astigmatism, or presbyopia, to prescribe corrective lenses if needed.
- Pupil Reaction and Eye Muscle Tests: Evaluates how the pupils respond to light and assesses eye movement.
- Visual Field Test: Identifies any loss of peripheral (side) vision, which can signal conditions like glaucoma or neurological problems.
- Slit Lamp Examination: Involves a microscope with a bright light to examine the structures of the eye, including the cornea, iris, lens, eye nerve and retina.
- Intraocular Pressure Test (Tonometry): Measures the pressure inside your eyes to screen for glaucoma.
- Dilated Eye Exam: Eye drops are used to dilate your pupils so that the specialist can thoroughly examine the retina and eye nerve for signs of damage or disease.
- Specialised tests: Advanced imaging techniques such as Optical Coherence Tomography (OCT) or retinal photography may be performed to get detailed images of the eye's structures.

Surgical Treatments
Eye specialists in Singapore use a range of surgical procedures to treat eye diseases. These surgeries include:
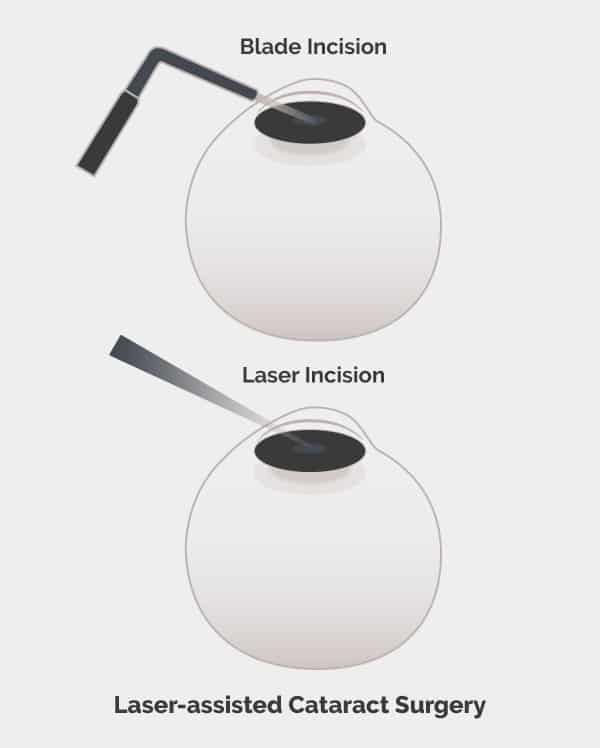
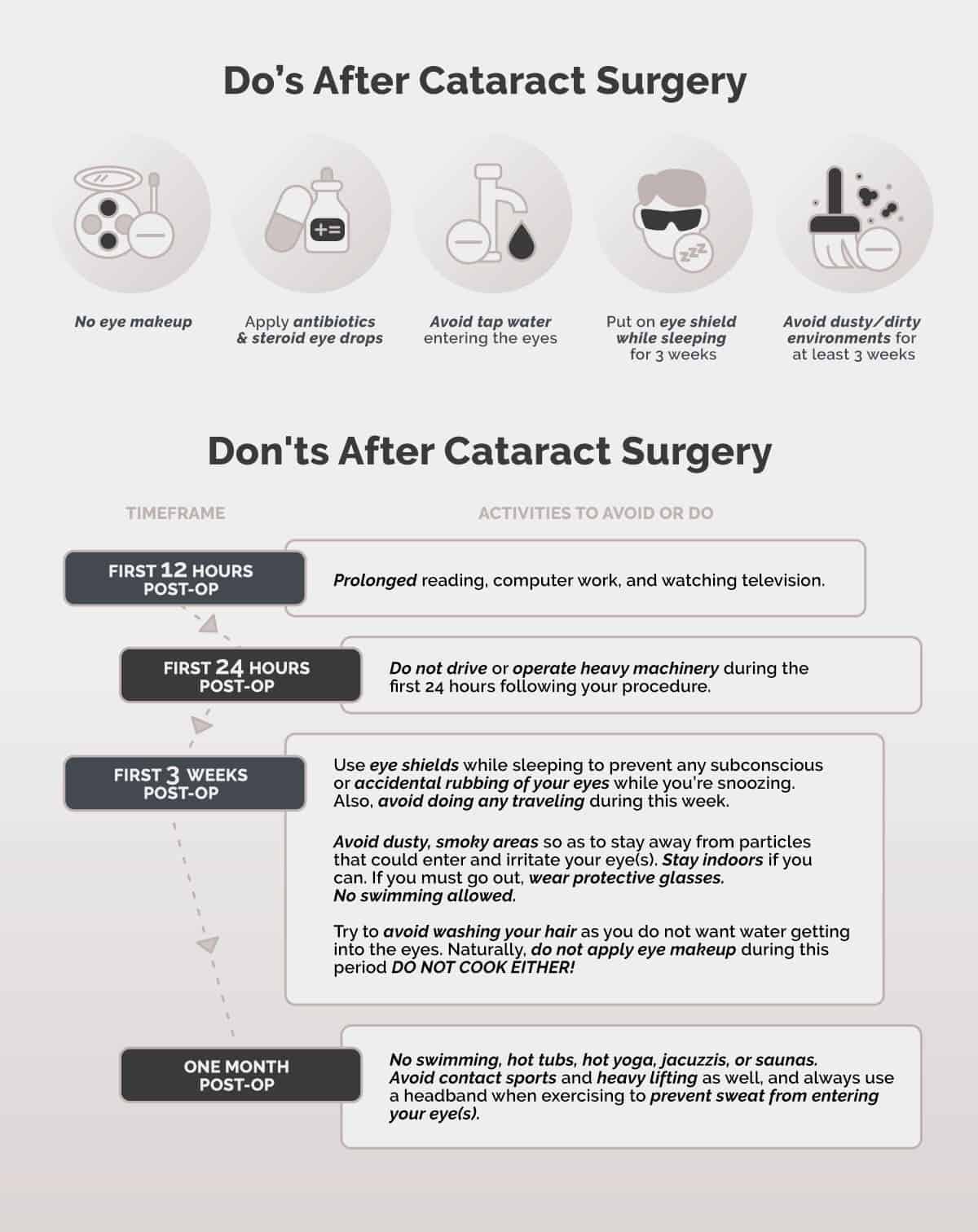
- Cataract Surgery: Cataract surgery involves removing a cloudy lens and replacing it with a clear artificial intraocular lens. This restores clear vision and may reduce dependency on spectacles.
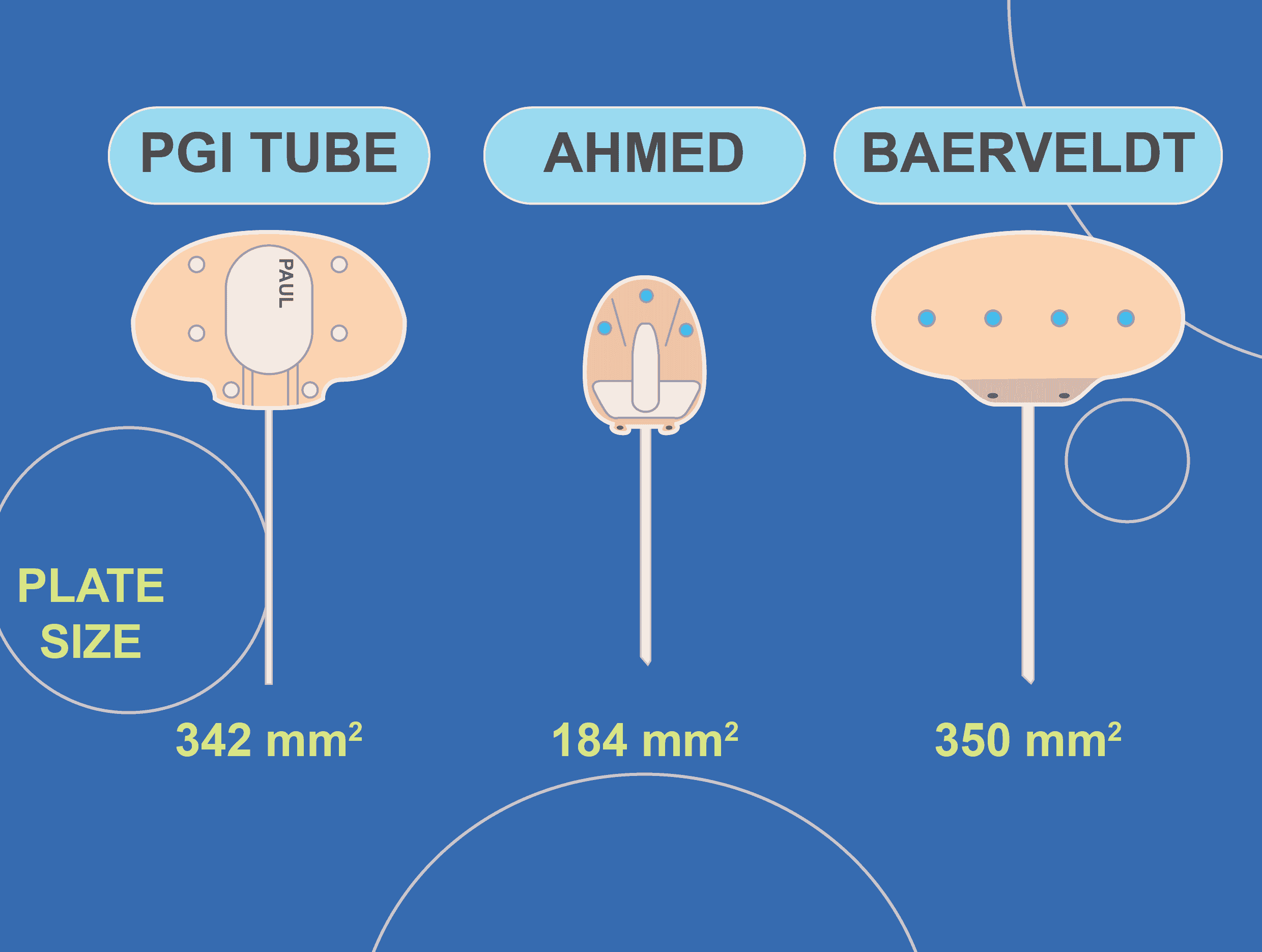
- Glaucoma Surgery: Glaucoma surgery aims to lower eye pressure to reduce further damage to the eye nerve. Glaucoma surgeries include trabeculectomy, tube implant surgery, minimally invasive glaucoma surgery and laser procedures.
- Retinal Surgery: Retinal detachment, macular holes, or diabetic retinopathy may require specialised procedures such as vitrectomy or laser photocoagulation to preserve or restore vision.
- Strabismus Surgery: Strabismus surgery corrects misaligned eyes by adjusting the eye muscles to improve one’s appearance and binocular vision.
- Eyelid Surgery: Ptosis surgery [3] and blepharoplasty address droopy eyelids or excess skin, enhancing both function and aesthetics.
Management of Eye Conditions
Ophthalmologists play an important role in diagnosing and managing sight-threatening eye conditions. These conditions often progress over time and may significantly affect vision and quality of life if not properly treated. Here are some examples of complex conditions and their management approaches:
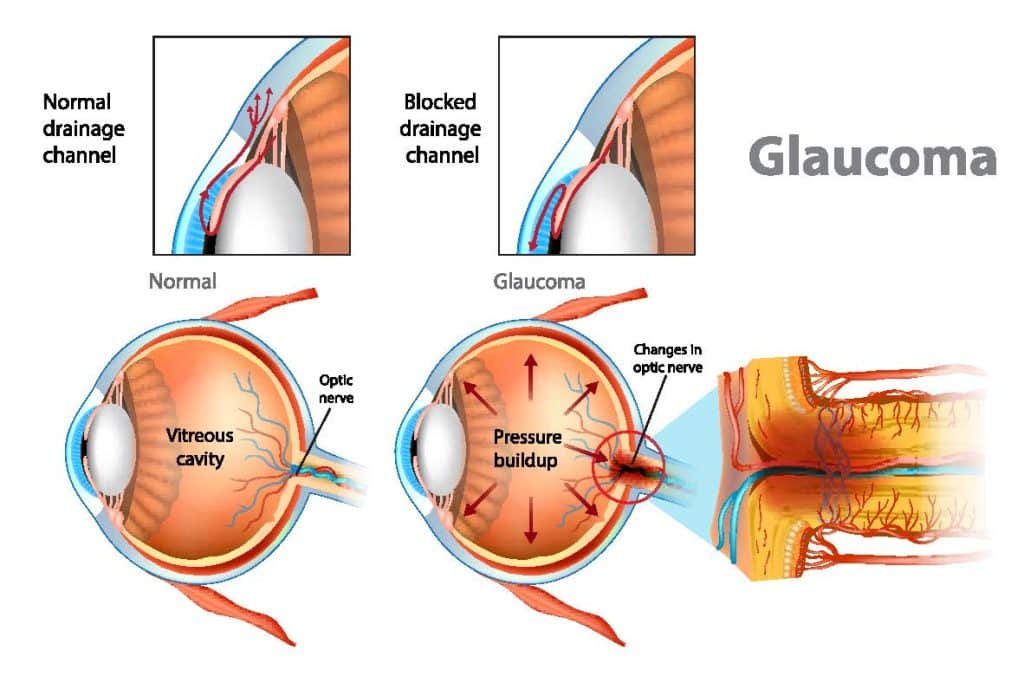
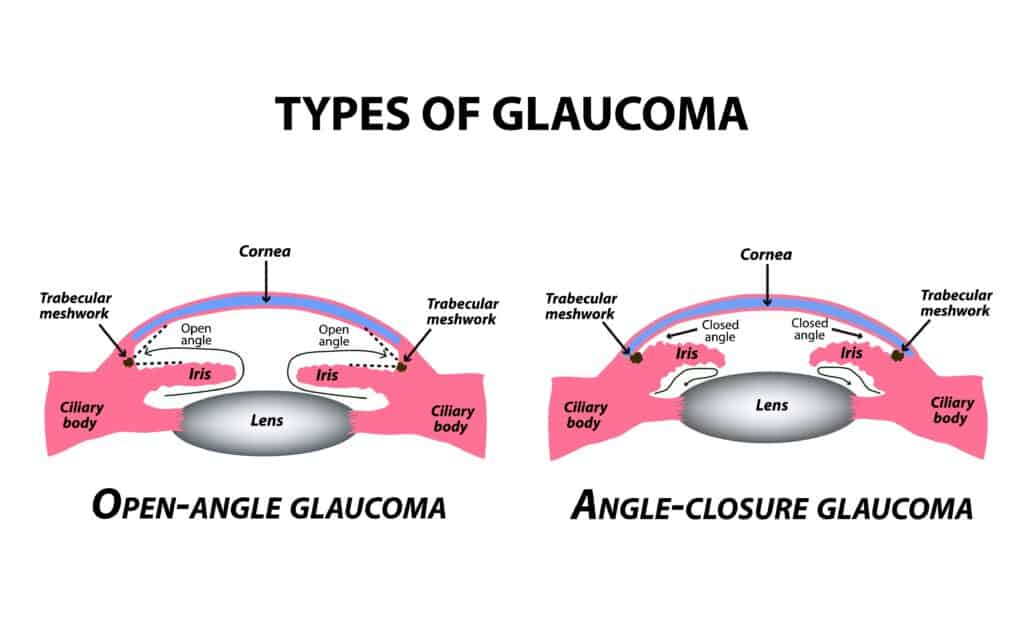
- Glaucoma: A group of diseases characterised by eye nerve damage, often due to high eye pressure. Management typically includes regular monitoring of glaucoma tests, medications to reduce eye pressure, and surgical procedures like trabeculectomy, tube implant surgery or minimally invasive glaucoma surgery (MIGS).
- Diabetic Retinopathy: Poorly controlled diabetes damages the blood vessels in the retina, resulting in irreversible visual loss in advanced cases. Management of this condition includes regular dilated retinal examination, laser treatments, and injections to reduce retinal swelling.
- Macular Degeneration: The deterioration of the central retina (macula) is a common cause of vision loss in older adults. When there is associated swelling of the macula due to leakage from abnormal blood vessels, anti-VEGF injections [4] are given to shrink the abnormal blood vessels and reduce macula swelling. Repeated injections long-term may be required to prevent further loss of vision.
- Corneal Diseases: Conditions like keratoconus or corneal scarring impair the cornea’s ability to focus light properly. Management includes corneal cross-linking, laser treatments, and corneal transplant.
- Pediatric Eye Disorders: Issues such as amblyopia (lazy eye) and strabismus (misaligned eyes) often develop in childhood. Management of these conditions involves customised treatment plans that may include surgeries or corrective lenses.
- Dry Eyes: This occurs when tear production is insufficient, when the tears evaporate too quickly, or when the tear composition is abnormal. There are many causes of dry eyes, including ageing, certain medications, lack of sleep, excessive screen time, environmental factors, and underlying conditions like autoimmune diseases or hormonal changes. Management includes artificial tears (eye drops or ointment) and punctal plugs (to block the drainage of tears to the nose, hence increasing the volume of tears on the ocular surface).
- Blepharitis: Inflammation of the eyelids, often caused by bacterial infection, result in eye redness, irritation, and sometimes eyelid infection. Management of blepharitis includes warm compress, eyelid hygiene, antibiotic ointments or eyedrops, topical steroid eye drops, and vitamin supplements.
Reasons to Visit an Eye Specialist in Singapore
Caring for your eyes is essential to maintaining optimal vision and preventing long-term complications. While some eye issues may seem minor, they can be early signs of more severe conditions. If you or a loved one are experiencing any vision changes or abnormal eye symptoms, it is best to see an ophthalmologist as early treatment can prevent irreversible damage.
Here are some situations where visiting an eye specialist is recommended:
- Routine eye examinations: Regular eye tests and check-ups are important to monitor any vision changes and catch issues early. For those over the age of 40 years, an eye review at least every 2-4 years is advisable, while for those over the age of 65 years, an eye review at least every 1-2 years is advisable. If you have a family history of eye diseases (eg. glaucoma), or if you have diabetes, an annual eye examination is recommended.
- Experiencing vision changes or problems: Those experiencing symptoms such as floaters, blurry vision, or difficulty seeing at night may have underlying conditions such as cataract, refractive errors, or retinal problems, and should see an eye specialist as soon as possible.
- Eye pain: Eye pain and discomfort such as redness and itchiness could signify eye infections, glaucoma, blepharitis, or other conditions.
- Eye injury or trauma: Injuries to the eye such as blunt trauma, chemical exposure, or scratches may heal on their own but can also cause lasting damage. Those who experience such eye injuries should visit an eye specialist to get an eye examination.
- Medical conditions: Those with chronic medical conditions such as diabetes should be monitored regularly by an ophthalmologist as they can lead to eye issues [5] such as diabetic retinopathy, diabetic macular edema, cataract, and glaucoma.
- Vision problems in children: Parents should pay attention to vision issues in children such as squints or difficulty reading as these may be a consequence of amblyopia (lazy eyes) or myopia.
When to Seek Immediate Attention from an Eye Specialist
Certain eye conditions can indicate a serious emergency that requires immediate medical attention. If you experience any of the following symptoms, it's crucial to consult an eye specialist as soon as possible:
- Sudden vision loss: Losing vision suddenly in one or both eyes can indicate serious issues such as retinal detachment, stroke, or a blockage in the blood vessels supplying the eye. Emergency intervention is essential to prevent permanent visual loss.
- Flashes of light or floaters: Seeing flashes of light or an increase in floaters (small spots or lines in your vision) could suggest retinal tears, retinal detachment or vitreous haemorrhage. These conditions require immediate attention to preserve vision.
- Severe eye pain: Severe, sharp, or persistent eye pain may be a sign of serious conditions, including glaucoma, an eye infection, or a foreign object in the eye. Immediate care is needed to prevent complications.
- Trauma or injury to the eye: Accidents or sports injuries can cause damage to the eye and the surrounding structures, requiring immediate medical attention
- Acute glaucoma [6]: A sudden increase in eye pressure can cause severe pain and irreversible vision loss if not treated immediately.
- Retinal detachment: A medical emergency where the retina separates from the back of the eye, leading to a potential loss of vision.

Choosing an Eye Specialist in Singapore
When selecting an eye specialist in Singapore, it’s important to consider factors such as credentials and experience. Ensure that the ophthalmologist is accredited by the Singapore Medical Council (SMC), which guarantees that the specialist has met the necessary standards to practice in Singapore.
Additionally, you should look for a specialist with experience in the specific area of your concern, whether it’s glaucoma, retina, or cornea. A specialist with advanced training who focuses on the latest treatments and technologies will be equipped to provide the best care for eye issues and conditions.
Dr Chelvin Sng is a qualified ophthalmologist in Singapore specialising in glaucoma, cataracts, and general ophthalmology. Known for her patient-centric approach, Dr. Sng uses advanced technology and offers personalised treatment plans to meet each patient's individual needs, ensuring optimal eye health outcomes. Contact us today to book an eye screening or appointment.
Cost of Visiting an Eye Specialist in Singapore
The cost of seeing an eye specialist in Singapore can vary between different clinics. On average, private clinics charge a consultation fee, in addition to charges for examination procedures and investigations. Higher fees may apply for specialist consultations requiring many diagnostic tests. Fees for consultation and investigations are generally lower at public hospitals, especially with subsidies for Singapore citizens and Permanent Residents, but waiting times for appointments may be longer.
If eye procedures are required, such as surgeries for cataract, glaucoma and retinal detachment, additional charges would apply. Eye clinics in Singapore typically charge within the Ministry of Health recommended guidelines for these procedures. Occasionally, the charges may exceed the Ministry of Health guidelines if the procedures are of exceptional complexity or if they are performed after-office-hours.
Eligible Singaporeans and Permanent Residents can use MediSave [7] for certain eye-related surgeries to offset the procedure costs. Many private health insurance plans also offer coverage for specialist consultations, diagnostic tests, and surgeries. It’s important to check the specifics of your plan for coverage details if you are required to undergo treatment for eye issues.
Preventative Eye Care Tips
Taking proactive steps to care for your eyes is essential in maintaining good vision and preventing potential issues as you age. While some factors like genetics may be beyond our control, adopting healthy habits can significantly reduce the risk of developing eye conditions.
Here are some tips to protect your vision, including strategies to reduce screen time, nutrition advice for maintaining eye health, and lifestyle adjustments. By incorporating these preventative measures into your daily routine, you can reduce eye strain, maintain good vision and improve your quality of life.
- Follow the 20-20-20 rule [8]: To reduce eye strain, every 20 minutes, look at something 20 feet away for 20 seconds. This gives your eyes a break and helps prevent fatigue caused by prolonged screen time.
- Ultraviolet light filters: Ultraviolet light filters and wearing hats to block the ultraviolet rays from entering the eyes can reduce the incidence of certain eye diseases, including cataract, pterygium and age-related macular degeneration.
- Healthy foods: A diet rich in vitamins A, C, E, omega-3 fatty acids, and antioxidants is essential for maintaining eye health. Foods like carrots, leafy green vegetables, fish, and nuts are excellent for preserving vision.
- Stay hydrated: Proper hydration is essential for maintaining tear production and preventing dry eyes. Drink plenty of water throughout the day.
- Regular exercise: Engaging in regular physical activity can help reduce the risk of conditions like high blood pressure and diabetes, both of which can affect your vision.
- Quit smoking: Smoking increases the risk [9] of developing eye diseases such as cataract and age-related macular degeneration (AMD). Quitting smoking significantly reduces these risks.

Conclusion
Timely and proactive eye care is vital for preventing long-term vision problems. Conditions like cataract, glaucoma, and diabetic retinopathy can develop slowly and without noticeable symptoms until the advanced stages of the disease. Regular eye checkups help detect such conditions early.
Even if you do not have any current eye issues, scheduling routine eye exams with a qualified ophthalmologist is essential. Be proactive about your eye health and visit an eye specialist regularly, especially if you are over 40, have a family history of eye disease, or experience symptoms such as blurred vision, eye discomfort, or sensitivity to light.
Frequently Asked Questions (FAQs)
How often should I visit an eye specialist?
For those over 40 years, an eye review at least every 2-4 years is recommended, and for those over 65 years, an eye review at least every 1-2 years is recommended. If you have risk factors (family history of eye diseases or conditions like diabetes), you should visit an ophthalmologist annually.
How should I prepare for an appointment with an ophthalmologist?
To prepare for an ophthalmologist appointment, it is advisable to bring any relevant medical reports, referral letters, and medications. If you wear contact lenses, you should stop wearing them for a few days before your appointment. If pupil dilation is required to examine the retina, avoid driving for 4-6 hours after the eye review and wear sunglasses to minimise glare.
How is an ophthalmologist different from an optometrist or optician?
An ophthalmologist is a medical doctor who can perform surgery and prescribe medications, while an optometrist provides eye exams, prescribes corrective lenses, and can diagnose certain eye conditions. An optician fits and dispenses eyeglasses and contact lenses based on prescriptions from an ophthalmologist or optometrist. Ophthalmologists, optometrists and opticians work closely together to help patients achieve the best vision and eye health.
Is eye surgery safe?
Modern eye surgeries, such as cataract removal, LASIK, or minimally invasive glaucoma surgery, are generally safe. However, as with any surgery, there are potential risks that your ophthalmologist will discuss with you before performing any procedure.
References
- Singapore National Eye Centre. (n.d.). Singapore’s eye health. Singapore National Eye Centre from https://www.snec.com.sg/giving/singapores-eye-health
- National University Hospital (NUH). (n.d.). Cataract. National University Hospital. Retrieved from https://www.nuh.com.sg/care-at-nuh/outcome-of-our-care/cataract
- Koka K, Patel BC. Ptosis Correction. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK539828/
- Kovach, J. L., Schwartz, S. G., Flynn, H. W., Jr, & Scott, I. U. (2012). Anti-VEGF Treatment Strategies for Wet AMD. Journal of ophthalmology, 2012, 786870. Retrieved from: https://doi.org/10.1155/2012/786870
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Diabetic eye disease. U.S. Department of Health and Human Services. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-eye-disease#:~:text=loss%20from%20diabetes%3F-,What%20is%20diabetic%20eye%20disease%3F,poor%20vision%20or%20even%20blindness.
- WebMD. (n.d.). Acute angle-closure glaucoma. WebMD LLC. Retrieved from https://www.webmd.com/eye-health/acute-angle-closure-glaucoma
- Ministry of Health Singapore. (n.d.). Medisave. Singapore Ministry of Health. Retrieved, from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/medisave
- Medical News Today. (2018, September 25). What to know about blepharitis. Medical News Today Retrieved from https://www.medicalnewstoday.com/articles/321536
- U.S. Food and Drug Administration. (2020, September 16). How smoking can contribute to vision loss and blindness. U.S. Department of Health and Human Services. Retrieved from https://www.fda.gov/tobacco-products/health-effects-tobacco-use/how-smoking-can-contribute-vision-loss-and-blindness